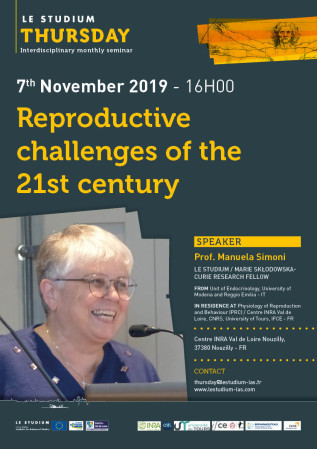
Prof. Manuela Simoni

From
Unit of Endocrinology, University of Modena and Reggio Emilia - IT
In residence at
Host scientist
Dr Pascale Crépieux
PROJECT
Pleotropism of Gonadotropin action
Evidence exist that the gonadotropins LH and FSH can substitute to each other under certain circumstances, in addition to the fact that they can act together in granulosa cells. In this project, our aim is to investigate how the two human gonadotropins influence each other in granulosa cells expressing both receptors, or by co-culturing cells expressing either the LHCGR or the FSHR (as a model granulosa/theca interaction). To reach this aim, we will use in vitro approaches to monitor cell signaling and steroid synthesis, as well as in silico modeling to gain insight onto the dynamics of the intertwined cell response to FSH and LH. Hypotheses about the underlying mechanisms will be proposed and tested through a systems biology approach combining computational modelling and experimental measurements. This project may open new possibilities for the pharmacological manipulation of FSH and/or LH in clinical practice, in order to improve infertility treatment, (multi)follicular growth for assisted reproduction, ovulation and spermatogenesis.
Publications
Follicle‐stimulating hormone (FSH) has been used in inconclusive clinical trials for male idiopathic infertility in the past. FSH is sometimes prescribed empirically for male idiopathic infertility, showing some improvement in sperm parameters in about half of the patients. In this opinion article, we briefly analyze the pathophysiological evidences in favor of a more aggressive approach in planning future studies on pharmacological FSH use in male infertility, in analogy with the FSH use for multiple follicular growth in women undergoing ovarian stimulation for assisted reproduction. There is sufficient evidence that spermatogenesis does not run at its top in the primate and that some extra FSH can stimulate spermatogenesis over its baseline. Existing data suggest that the pharmacological regimens applied so far were insufficient, both in dosage and in duration, to elicit this response in about half of the patients. A paradigm change is needed now: We should move away from the classical, endocrinological approach, which simply applied the substitutive, therapeutic regimen used in hypogonadotropic hypogonadism, toward testing a ‘testicular hyperstimulation’ scheme for a time sufficient to cover more than only one spermatogenic cycle, a concept to be verified in an appropriately controlled, prospective, randomized clinical trial.
Recombinant follicle-stimulating hormone (FSH) (follitropin alfa) and biosimilar preparations are available for clinical use. They have specific FSH activity and a unique glycosylation profile dependent on source cells. The aim of the study is to compare the originator (reference) follitropin alfa (Gonal-f®)- with biosimilar preparations (Bemfola® and Ovaleap®)-induced cellular responses in vitro. Gonadotropin N-glycosylation profiles were analyzed by ELISA lectin assay, revealing preparation specific-patterns of glycan species (Kruskal-Wallis test; p < 0.05, n = 6) and by glycotope mapping. Increasing concentrations of Gonal-f® or biosimilar (1 × 10−3-1 × 103 ng/ml) were used for treating human primary granulosa lutein cells (hGLC) and FSH receptor (FSHR)-transfected HEK293 cells in vitro. Intracellular cAMP production, Ca2+ increase and β-arrestin 2 recruitment were evaluated by BRET, CREB, and ERK1/2 phosphorylation by Western blotting. 12-h gene expression, and 8- and 24-h progesterone and estradiol synthesis were measured by real-time PCR and immunoassay, respectively. We found preparation-specific glycosylation patterns by lectin assay (Kruskal-Wallis test; p < 0.001; n = 6), and similar cAMP production and β-arrestin 2 recruitment in FSHR-transfected HEK293 cells (cAMP EC50 range = 12 ± 0.9–24 ± 1.7 ng/ml; β-arrestin 2 EC50 range = 140 ± 14.1–313 ± 18.7 ng/ml; Kruskal-Wallis test; p ≥ 0.05; n = 4). Kinetics analysis revealed that intracellular Ca2+ increased upon cell treatment by 4 μg/ml Gonal-f®, while equal concentrations of biosimilars failed to induced a response (Kruskal-Wallis test; p < 0.05; n = 3). All preparations induced both 8 and 24 h-progesterone and estradiol synthesis in hGLC, while no different EC50s were demonstrated (Kruskal-Wallis test; p > 0.05; n = 5). Apart from preparation-specific intracellular Ca2+ increases achieved at supra-physiological hormone doses, all compounds induced similar intracellular responses and steroidogenesis, reflecting similar bioactivity, and overall structural homogeneity.
Editorial on the Research Topic.
Propagating life to the next generation is a hormone-dependent process relying on the individualwish to generate own progeny and resulting in maintenance of species. This Research Topicis dedicated to Follicle–Stimulating Hormone (FSH) and itsreceptor (FSHR) and their rolein reproduction. FSH is a typical example of a drug which entered clinical use in the “pre-evidence-basedmedicine era,” just for its efficacy in stimulating gonadal function and fertility in hypogonadotropichypogonadism. More recently, FSH entered clinical use in controlled ovarian stimulation in orderto obtain multiple follicular growth for assisted reproduction. Given the progressive increase incouple infertility, the demand for assisted reproduction grows steadily and the FSH market isflourishing. Yet, very little was known about the FSH mode of action until a few years ago,and the therapeutic use of FSH is still far from being evidence-based. But great progress in ourunderstanding of FSH action was made in the last two decades and, since not many scientistsaround the world are active in the gonadotropin/FSH research “niche,” we thought it was time tocall them to report to tell us their view on the state-of-the-art. The result is this “Research Topic.”
Commercial gonadotropin-releasing hormone (GnRH) antagonists differ by 1–2 amino acids and are used to inhibit gonadotropin production during assisted reproduction technologies (ART). In this study, potencies of three GnRH antagonists, Cetrorelix, Ganirelix and Teverelix, in inhibiting GnRH-mediated intracellular signaling, were compared in vitro. GnRH receptor (GnRHR)-transfected HEK293 and neuroblastoma-derived SH-SY5Y cell lines, as well as mouse pituitary LβT2 cells endogenously expressing the murine GnRHR, were treated with GnRH in the presence or absence of the antagonist. We evaluated intracellular calcium (Ca2+) and cAMP increases, cAMP-responsive element binding-protein (CREB) and extracellular-regulated kinase 1 and 2 (ERK1/2) phosphorylation, β-catenin activation and mouse luteinizing-hormone β-encoding gene (Lhb) transcription by bioluminescence resonance energy transfer (BRET), Western blotting, immunostaining and real-time PCR as appropriate. The kinetics of GnRH-induced Ca2+ rapid increase revealed dose-response accumulation with potency (EC50) of 23 nM in transfected HEK293 cells, transfected SH-SY5Y and LβT2 cells. Cetrorelix inhibited the 3 × EC50 GnRH-activated calcium signaling at concentrations of 1 nM–1 µM, demonstrating higher potency than Ganirelix and Teverelix, whose inhibitory doses fell within the 100 nM–1 µM range in both transfected HEK293 and SH-SY5Y cells in vitro. In transfected SH-SY5Y, Cetrorelix was also significantly more potent than other antagonists in reducing GnRH-mediated cAMP accumulation. All antagonists inhibited pERK1/2 and pCREB activation at similar doses, in LβT2 and transfected HEK293 cells treated with 100 nM GnRH. Although immunostainings suggested that Teverelix could be less effective than Cetrorelix and Ganirelix in inhibiting 1 µM GnRH-induced β-catenin activation, Lhb gene expression increase occurring upon LβT2 cell treatment by 1 µM GnRH was similarly inhibited by all antagonists. To conclude, this study has demonstrated Cetrorelix-, Ganirelix- and Teverelix-specific biased effects at the intracellular level, not affecting the efficacy of antagonists in inhibiting Lhb gene transcription.
Final reports
Evidence exists that the gonadotropins LH and FSH can substitute to each other under certain circumstances, in addition to the fact that they can act together in granulosa cells. The aim of this study is to investigate how the two human gonadotropins influence each other in granulosa cells expressing both receptors, or by co-culturing cells expressing either the LHCGR or the FSHR (as a model granulosa/theca interaction). Plasmids encoding the c-myc-tagged-LHCGR and the FLAG-tagged FSHR under the control of an inducible coumermycin-responsive or doxycycline-responsive promoter, respectively were produced. These plasmids were used to permanently transfect human granulosa cell-derived KGN cells and HEK293 cells. The following cell lines were obtained and partially characterized: #1 c-myc-tagged-LHCGR-KGN; #2 FLAG-tagged FSHR_HEK293; #3 FLAG-tagged FSHR-KGN; #4 Double, c-myc-tagged-LHCGR and FLAG-tagged FSHR-KGN. After induction of receptor expression, the cell lines #1 and #2 and #3 responded to hCG and FSH stimulation, respectively by producing cAMP. Receptor expression was demonstrated by RT-PCR and flow cytometry. The characterization of the cell line #4 is ongoing. These cell lines are now available for the study of cell signaling and steroid synthesis, as well as in silico modeling, to gain insight into the dynamics of the intertwined cell response to FSH and LH in granulosa cells. These experiments will continue in parallel in both laboratories involved. Our cell lines represent new, very valuable instruments for the study of molecular pharmacology of FSH and LH, in order to improve infertility treatment, (multi)follicular growth for assisted reproduction, ovulation and spermatogenesis.